Andi Orlowski, Director of The Health Economics Unit hosted by NHS Midlands and Lancashire, and Dr Steven Laitner, General Practitioner and Freelance Health Consultant, discuss the importance of primary care networks supporting the well population as well as those with known ill health.
If a tree falls in the forest and no one is around to hear it, does it make a sound? And if a person doesn’t call their GP practice, are they still in good health?
The first question is philosophical; the second is a real one that population health management (PHM) is increasingly seeking to address – how primary care can support those people who might be well now, but are moving unseen and unknowingly towards ill health in the future.
Preventing ill health in the currently well population
Over the last few years, a growth in the use of PHM has increased the focus on the wider determinants of people’s health and wellbeing. However, there remains a tendency to focus on those people most at risk of hospital admission, and on those with more on complex needs. That’s in a way much more straightforward than working with the people who simply aren’t engaging with GP services, and ‘planning for the people you might see tomorrow’. That’s in the territory of the unknown unknowns!
The remit of primary care networks (PCNs) includes the prevention of ill health, and the new network contract includes a number of incentives related to early detection of cancer, CVD case finding and social prescribing to improve wellbeing, among others. So, while the NHS continues to deliver on its core mission of treating the unwell, PCNs also need to develop interventions to ensure that everyone gets the help and support that’s right for them, including the currently well population.
Personalised care within a PCN area
By segmenting a population into distinct groups, PCNs can begin the process of delivering personalised care at the levels of the three Ps – Place, Population Cohort and Person.
The three Ps are all about recognising that the place we live is part of who we are and has an impact on our health; there are also groups of people in that place with similar characteristics, for example the frail elderly, but within each group are unique individuals.
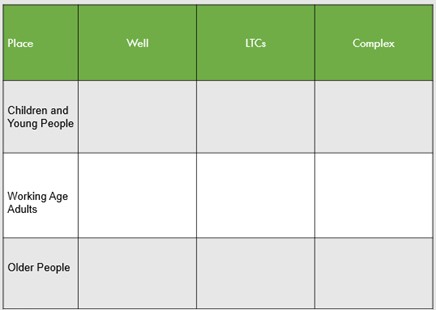
A segmentation tool such as the one below can be used at a place level to identify population cohorts, giving PCNs a starting point for PHM and personalising care for their population.
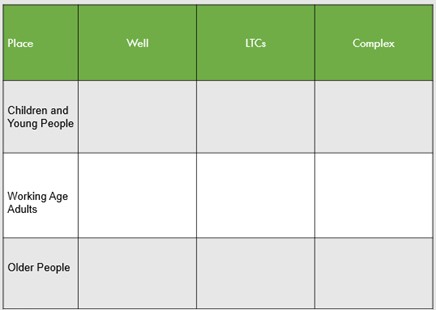
Ref: Created by Dr Steven Laitner and Dr Mark Davies, National Association of Primary Care
Well – No identified long-term condition. Normal nationally approved screening, immunisation, health promotion and disease prevention measures will apply.
LTCs – One or more long-term condition(s) requiring some form of ongoing care, support, management, treatment monitoring etc.
Complex – A complex mix of the following – physical, mental health and functional needs requiring ongoing multidisciplinary, proactive, highly personalised care.
To complete the grid, PCNs can access practice data across their network and call on local partners such as community and mental health trusts, social care and hospitals for additional patient-level data. They can also interact with their local integrated care system or integrated care providers to share data and better understand their population.
However, such data is biased towards the people who are already ill, as they are the ones we predominantly collect data on. If people haven’t engaged with the health system, how do we know about their health risks? The real challenge is working out how the health of the well population may have changed since they were last seen.
This is where social determinants such as school attendance, bin collection arrangements, free school meals and environmental factors may come into play. Public Health England’s fingertips tool – a free data repository of public health profiles – also provides a wealth of information on smoking levels and vaccination rates for example, and allows PCNs to benchmark themselves against the regional or England average on a number of indicators. The Office of National Statistics also publishes a wealth of information on wider determinants. Also, GPs hold much patient-level data on people’s BMIs, smoking data, alcohol intake, recent bereavements, domestic violence, children in need and other social factors. But how much of this data is proactively acted upon?
Understanding and serving whole populations
PCNs and GPs have much of the data they need to hand and can relatively easily case-find people with risk factors for future health problems. Primary care colleagues have many communication tools to reach out to their populations – telephone, text, email and so on, which allow them to reduce the risks by offering tailored support and interventions. Combining this with health coaches, care coordinators and social prescribing link workers to further personalise the support and finding interventions that the patient is amenable to receiving, offers the greatest chance of preventing a negative outcome.
PCNs were created to tailor interventions based on their deep understanding of their populations and their ability to care for themselves. Part of this is ensuring that the range of interventions stops everyone moving up the risk pyramid, not just the unwell people that GPs see.
Population health management allows PCNs to understand their place, to find people in different population cohorts, design cohort-tailored interventions then, of course, personalise care for each individual. It doesn’t need complex analysis – it’s very easy for PCNs to do at a simple level with a small investment of time. Maybe the first and hardest step is wanting to do something?
Find out more
To find out more about delivering PHM within a primary care network, please contact:
Andi Orlowski, Director of The Health Economics Unit – andi.orlowski@nhs.net
Dr Steven Laitner, General Practitioner and Freelance Health Consultant – steven.laitner@nhs.net
Follow the latest updates from the Health Economics Unit on LinkedIn and Twitter